Interscalene Block: Nerve Block for Shoulder Surgery
Interscalene Brachial Plexus Block
Interscalene blocks are used to relieve pain during and after surgery on the shoulder. The interscalene block is included in the category of regional anesthesia and is one of the most commonly used types of peripheral nerve blocks. First, here are the relevant definitions to make it easier to follow the medical-speak:
- Regional anesthesia: refers to the technique of numbing a large area of the body by injecting numbing medicine (local anesthetic) around a nerve or group of nerves that supply that area of the body. Sometimes epidurals and spinals are included in the category as they numb the lower half of the body.
- Peripheral nerve block: essentially the same as regional anesthesia but specifically excludes epidurals and spinals. "Peripheral" refers to nerves outside of the central axis of the nervous system (brain and spinal column).
- Interscalene block: numbing the nerves that supply the shoulder by injection of local anesthetic around the base of those nerves in the side of the neck.
Note
Although the author is a board-certified physician anesthesiologist, this article is not intended to provide medical diagnosis or advice. The content of this article is for general information only.
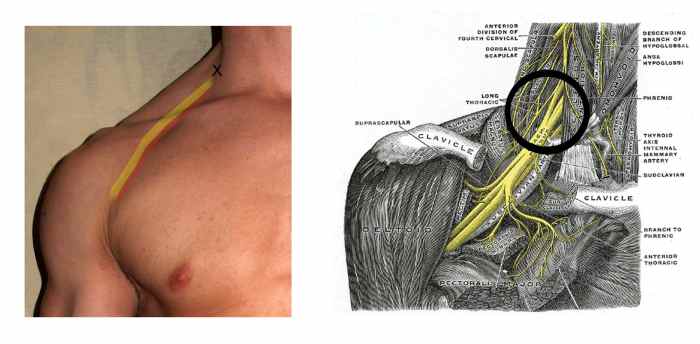
The X in the photo marks the site of injection for an interscalene block, while the diagram shows the target area.
By David Shankbone (Foto), Grey's anatomy. [GFDL (www.gnu.org/copyleft/fdl.html) or CC-BY-SA-3.0-2.5-2.0-1.0 (www.creativecommons.org/licenses/by-sa/3
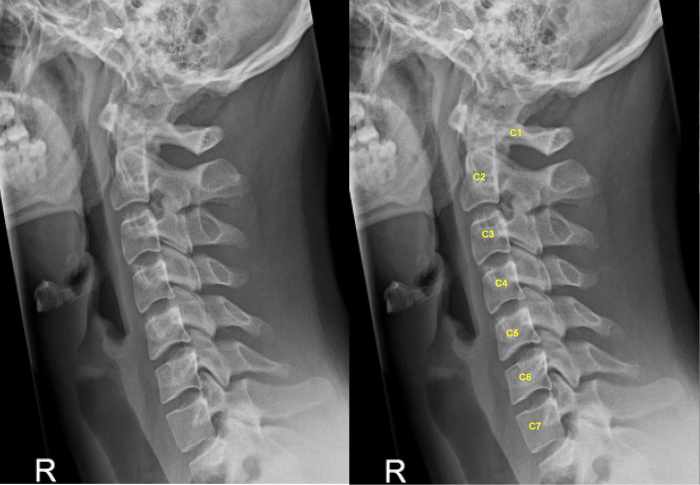
Lateral (from the side) X-ray of the cervical spine showing the number of the vertebrae, C1 to C7.
By Lucien Monfils (Own work) [GFDL (www.gnu.org/copyleft/fdl.html) or CC-BY-SA-3.0-2.5-2.0-1.0 (www.creativecommons.org/licenses/by-sa/3.0)], via Wiki
Brachial Plexus Anatomy: The Basics
The brachial plexus is a complex conglomeration of nerves in the upper neck and shoulder area. Nerve endings leave the upper spinal cord, join together, branch apart, divide, and eventually spread out into the individual nerves that travel out to provide sensation and movement to the shoulder and arm.
The vertebrae (backbones)—and the nerves that exit the spinal cord near them—are grouped by location:
- 7 cervical at the top of the neck (designated C1 to C7)
- 12 thoracic from the top to the low back (T1 to T12)
- 5 lumbar in the low back (L1 to L5)
- Then the sacrum and coccyx at the level of the hips and tailbone
The nerves at the origin of the brachial plexus come from the cervical spine, at levels C5, C6, C7 and the first thoracic vertebrae, T1.
A review of the detailed and complex anatomy of the brachial plexus is well beyond the scope of this article. As a quick summary, those cervical and thoracic nerves combine to form nerve trunks, and the trunks become divisions, with some of the original nerve fibers staying together and some splitting up. Then again, the divisions become cords and then branches which become the peripheral nerves providing sensation and movement to the arms.
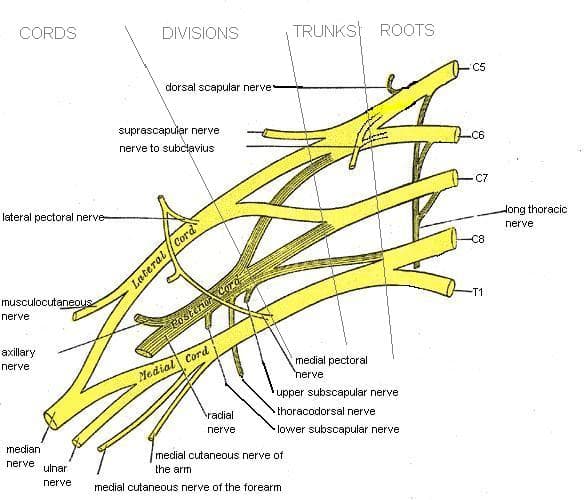
Diagram showing the brachial plexus. Note the combinations and divisions that end up becoming the nerves of the shoulder, arm and hand.
By Mattopaedia at en.wikipedia [Public domain], from Wikimedia Commons
Interscalene Block
The key to understanding how to perform an interscalene block and what to expect from it lies in this complicated anatomy. Injection of the numbing medicine must occur at a place that is accessible and effective for the purpose intended.
Your anesthesiologist has been trained in this technique. The injection will be done with either the nerve stimulator technique or with ultrasound guidance. Either way, you will likely be lightly sedated for the procedure and may or not remember parts of it later.
As with other peripheral nerve blocks, patients say it "feels funny" when the nerve stimulator is used (it makes the muscles twitch), but I've not had anyone say that it hurts to have it done.
Remember that the duration of action of the interscalene block is about 8 to 24 hours, with the average being maybe 10 to 12 hours. The interscalene block will not eliminate the need for pain pills (or intravenous medicine if you stay in the hospital). It will decrease the amount you need the first day and delay the hour at which you start taking them. This can be helpful to reduce pain during the drive home from the hospital, but you will likely still need pain meds that evening, night or early the next morning.
Recommended
Technique
As stated, the block is done either with a nerve stimulator or by ultrasound guidance. Either way, you will likely receive some sedation and be placed on a monitor for your EKG, blood pressure and oxygen levels to be measured. The neck will be cleaned with antiseptic soap, and you will be asked to turn your head away from the side getting the block. You may be asked to lift your head or tense your neck muscles briefly to help identify the muscular landmarks used to do the block.
The big muscle running down and diagonally toward the front of your neck is the sternocleidomastoid. Behind this are the scalene muscles. There is a groove between the anterior and middle scalene muscles. This is the interscalene groove and is the site of injection for this block.
Local anesthetic is usually given to numb the skin where the injection will go. The needle is passed just a centimeter and no more than two into the correct spot on the side of the neck. If a nerve stimulator is used, your arm will start to twitch but will stop in a few seconds after the anesthesiologist starts to inject the numbing medicine.
What to Expect From an Interscalene Block
- Numb shoulder
- Some arm numbness—be careful around hot or cold items; you may not feel burn or damage from temperature extremes
- Heavy, weak arm that may be difficult to lift up and away from the body
- Usually 8 to 24 hours of pain relief (average may be around 12 with currently used medications)
- Maybe Horner's syndrome
- Maybe some feelings of shortness of breath
What Is the Effect of the Interscalene Block?
When the brachial plexus is blocked by the interscalene technique, it can be expected to provide anesthesia or analgesia to the shoulder joint and overlying structures.
This block is performed at the level of C6, which is approximately the level just below the Adam's apple in the neck. The block numbs those parts of the shoulder innervated by the nerves originating from C5 to C7.
Functionally, this results in reliable numbing of the shoulder area. Some parts of the upper and lower arm will be numb, but the hand will not. For this reason, interscalene blocks are only recommended for shoulder surgery. It will be difficult to raise the arm from the shoulder as the arm will feel heavy and weak.
Side Effects
Horner's Syndrome
A side effect that may be expected (but may or may not occur) is Horner's syndrome. This is a condition caused by the blockade of sympathetic (part of the autonomic nervous system) nerve fibers involved in the interscalene block. I find this occurs in fewer than one in ten patients receiving this type of block. It is not considered a complication and is a normal variant of the block. It will resolve as the block wears off.
The resulting symptoms occur on the same side as the block and include:
- Ptosis: This is drooping of the eyelid
- Miosis: Constriction (making smaller) of the pupil
- Anhidrosis: Lack of sweating
Diaphragm Paralysis
The diaphragm (breathing muscle under the lungs) is innervated by the phrenic nerve. The phrenic nerve is supplied by C3, C4 and C5 nerve roots. Therefore, the phrenic nerve and the breathing muscle on the side of the block are paralyzed by an interscalene nerve block. This sounds really bad and dangerous, but unless you have severe lung disease, it usually doesn't create a problem. This nerve is blocked 100 percent of the time when a successful block is placed.
You should know that you may or may not notice a strange feeling of not being able to take a deep breath until the block wears off. Your cough may or may not feel weak. Most people do just fine, with the other side of the diaphragm functioning normally. Oxygen level is not usually affected, and this is of no clinical consequence in most people.
Hoarse Voice and Difficulty Swallowing
Because one of the nerves to the larynx (the recurrent laryngeal nerve) may be blocked by normal spread of the local anesthetic, a temporary hoarse voice may also result. Like the above side effects, this is not a complication or a problem, just a normal variant of the block that happens sometimes. Difficulty swallowing may or may not accompany this side effect.

Notice how the patient's left eye seems to be more closed due to the drooping eyelid (ptosis), and the pupil (black center) of the eye is smaller (miosis) in Horner's syndrome. This is a normal reaction that can occur with interscale.
By Waster [CC-BY-2.5 (http://creativecommons.org/licenses/by/2.5)], via Wikimedia Commons
Complications
Anytime an injection or medicine is given, there are potential complications. This is to be expected since the purpose of the intervention is to change something about how the body works. An interscalene block is no exception.
Complications can occur as a result of the medication, the needle used or both. These may be more likely in people with certain pre-existing conditions.
The neck has a dense concentration of structures that are important structures. The brachial plexus is only one of them. Other nerves, such as the carotid artery, the jugular veins, the spinal column, the epidural space, the windpipe . . . these are all structures near the injection site for interscalene block. Obviously, injection into one of these structures can be catastrophic.
Injections always have a risk of infection or bleeding. Because the blood vessels in the neck are large and important, causing injury to one is potentially dangerous. Luckily, this complication is rare.
If local anesthesia is injected into blood vessels, seizures, cardiac collapse, and even death can occur. This also is very rare.
Drops in blood pressure and heart rate have been reported due to reflexes that affect the part of the nervous system that controls these functions.
Injury to nerves, with or without warning during the procedure, can occur. In other words, some people have reported either temporary or permanent nerve injury after getting a seemingly perfectly performed interscalene block. Most of the time, if numbness or tingling persist after the block has worn off, it will resolve itself over, at most, a few months. Rarely, the nerve damage can be severe or permanent.
It is difficult to find reliable data on the exact percentages of these occurrences due to differences in reporting or accurate identification of the problem. The risk of any complication from interscalene block has been estimated to be anywhere from 5 to 20 percent. The more serious the complication, the rarer it is.
If you are having shoulder surgery, talk to your surgeon and anesthesiologist about your particular needs and risks, as there is a lot of variability from case to case.
Personally, this author uses them for total shoulder replacement and open rotator cuff repairs, most of the time and quite rarely for any arthroscopic surgery (through the scope) on the shoulder. I work with some surgeons who believe the risk is too high and request that their patients never have them, and some surgeons who request most of their patients get them.
This content is for informational purposes only and does not substitute for formal and individualized diagnosis, prognosis, treatment, prescription, and/or dietary advice from a licensed medical professional. Do not stop or alter your current course of treatment. If pregnant or nursing, consult with a qualified provider on an individual basis. Seek immediate help if you are experiencing a medical emergency.
Comments
Bobbie on May 31, 2020:
I recently underwent rotator cuff surgery repair. The anesthesia doctor used a block peripheral: interscalene. After post op and resting a day at home,swelling began on the non-operative side of my body. This was noticed in my feet and toes. It has lasted a couple of weeks and until my next visit. Does the procedure cause this complication?
Other DOC on September 06, 2019:
I want to know if Tahoe doc puts blocks in before the surgeon arrives at the facility?
If so, is there legal exposure if something goes awry during a block and the surgeon is not even at the facility?
Never again on June 27, 2019:
I had arthroscopic surgery to repair 3 completely torn rotator cuff tendons and a completer tear of my bicep muscle. I remember waking up in pain during the surgery and hearing someone say "she's back." My 2 hour recovery time became a 7 hour recover time. I had a horrible time breathing and felt like I was gasping for air. I was extremely out of it and have some memories of the nurses discussing whether I was going to be admitted. A pulmonary specialists was called to give me a breathing treatment. I remember him telling the nurses that this should not have happened. I remember being thrown into my clothes like a rag doll and have no idea how I got into the car to go home. It took 10 days for my head to clear. No one would tell me anything. I have a friend that works in an OR and they were able to look at my records and tell me what had happened. I had gone into V-tech and they immediately stopped all anathesia which is why I woke up. I was then given large does of several types of anethesia to knock me out again. My diaphragm was paralyzed and I could not breathe. I was also given several drugs to combat an opioid overdose. My throat was raw, I was gasping for air, coughing, and extremely thirsty (a side effect of the opioidd reversal drugs.) The doctors and nurses would not tell me what happened, I was lucky to have someone to go to. I have two partially torn rotator cuffs in my other shoulder and the surgeon wants to fix them as well. I am going to try physical therapy first and will never have another nerve block to my shoulder again. I feel the risks are too high.
I underwent shoulder replacemen surgery with block on January 22, 2019:
I chose a teaching hospital for my procedure, primary total shoulder replacement I watched the intern through the block procedure because she was guided by ultrasound. The resident continuously directed her so she took time to perform it.
I felt great afterwords and went home day of surgery. I was the first patient in the surgeon's 35 year career who went home the same day. I have a very high pain threshold. I needed pain medications the first day. I abstained afterwards.
Larry Deyton on June 22, 2018:
I was given the nerve block for arthroscopic shoulder surgery (spur and frozen shoulder). It was left and and I was discharged with the wire still attached with a container with medicine at the end that would "feed" my neck through the wire (taped well). After three days I removed it as directed. All was good until day 8 post-surgery where I had a serious dull pain in my shoulder, followed the next day with severe burning in my deltoid muscle with certain movements. The outer layer of my shoulder (below the joint and half way down my upper arm) became numb. It has been 2.5 months post-surgery and numbness exactly the same and the burning has decreased from a score of "9" to around a "3" or so. I can adjust to a numb shoulder but the reason for the burning is likely tied to the tendons/muscle that make up the deltoid is constricted (tightened) which remains constantly sore. A concern I have is with those tendons being so tight (a constant feeling as if I am always in a state of lifting something heavy) is that when I do exercise it I may be at risk of tearing it. The soreness is also where the muscle meets the mid arm bone. I wish I had known the risks, as I have zero recollections of being given an option, only explained what the block was going to do by the anesthesiologist. I am worse off than before I had surgery.
Lin on May 06, 2018:
I had rotator cuff repair 2 weeks ago and had the shoulder block and catheter inserted for 3 day pain relief. After being home for 1.5 hours I awoke to drooping eye lid, numb throat, difficult speaking, and swollen face. Went to ED and was admitted to rule out stroke or brain bleed. The infusion was also stopped. After 2-3 day hospital stay it was determined that I may have had horner's syndrome from block. I now still have numbness to a small section in my scalp and something strange happening to my 2 fingers. I say all this to make folk aware that these symptoms may occur but they were no where listed as a side effect when I left to go home initially. I think patients need to be monitored longer than 30 minutes after a block. Life vs time.
Michael A Hall on February 06, 2018:
Had one done for rotator cuff and bicep repair surgery a week ago. I believe I got a "double" dose as the Dr called for 20cc's of something twice. The first 20cc's didn't have the desired numbing effect. After the second dose started taking effect I couldn't breathe; which put me in a full blown panic attack. It wasn't "shortness of breath", it was I couldn't breathe! It got worse when I got into the OR. If I ever have to do another shoulder surgery I will either forgo the block or request something for the anxiety before they do it.
Cindy Dances on November 30, 2017:
I had shoulder surgery 8 weeks ago and my interscalene block lasted 28 hours. When the pain started it was excruciating and lasted for almost 2 weeks. I was glad to have that one day of pain relief to get settled in at home and get medications picked up. I can say that the surgical pain that I experienced for 2 weeks could cause strain on my heart more than the block that I had. After reading several comments below, I had to put my positive input here. It seems like we only read the bad reviews.
Joyce on August 30, 2017:
I had the nerve block 4 weeks ago. Immediately I could not take a deep breath. It was terrifying and nobody would tell me what was going on until after surgery and then I had to beg. I am going to the doctor in a few minutes because I have had a terrible sore throat with blisters, choking and difficulty swallowing. I had great success with my rotator cuff surgery; however, I will never have another nerve block for my arm. I had two at Duke for knee replacement and did great.
vallaug on June 08, 2017:
I am facing total shoulder replacement at a facility that uses this block and from the information here, I would want to refuse it. what other pain management methods can be used?
Melody on June 05, 2017:
I had rotator cuff surgery a year ago and one month after I had two heart attacks and I'm wondering if the block was the cause there is no history of heart problems In my family.
Judy on March 10, 2017:
It's been a little over three weeks since my shoulder surgery and I have nerve damage from the block. Never again! I am right-handed and it's my right arm and hand which are affected. I'm terrified that I won't regain full function of my hand and arm again.
Sandra lucas on November 20, 2016:
I've had intervene lock twice, five months apart. Vastly different results. The first I barely remember receiving and the block lasted over 24 hours. The second one I was awake throughout the procedure and there was some discomfort when the nerve was touched. When I woke up I had all the symptoms you mention...breathing abnormalities, throat felt raspy, eyelid drooped. The night I got home I developed a nice shinier...still have it after 5 d days. Abnormal?
Kathy McGraw from California on September 06, 2014:
I had some sort of block for radial head surgery but don't know if it was this kind. However I had a tube in my shoulder area that was supposed to be a block that if the pain was too much I would just press a button. I had to have it removed as it didn't appear to work and the Ortho guy said maybe it was in the wrong spot? Anyway....thank you, very interesting to read from a professional.
Melissa on August 08, 2014:
My father recently had rotator cuff surgery and had the block and now he has a paralyzed right diaphragm. Is this normal and will it heal?
The doctor said it was from the pain pump, is that possible?
teamrn from Chicago on April 14, 2014:
The three times I've had nerve blocks, all at pretty established hospitals, I wasn't given a choice, though 2 times I spent considerable time discussing with my anesthesiologist-so, I guess I was given a choice, but because of certain conditions, other options were taken off the table. I believe it was surgeon preference. But, you (as the anesthesiologist) would have the final say, so, wouldn't you?
TahoeDoc (author) from Lake Tahoe, California on April 14, 2014:
Yes. I still sometimes do the block for shoulder replacements or other open/non-arthroscopic surgeries. But, it really depends on the person, their preference, surgeon preference, other medical conditions, etc. Also, I work in a hospital where we do a fair number and our other methods of pain relief are pretty well set up, so even that is becoming less frequent.
teamrn from Chicago on April 13, 2014:
Is there a difference in the need for an inter scalene block when you have a HHR and perhaps a reverse shoulder. I should think the reverse shoulder would still need it.
TahoeDoc (author) from Lake Tahoe, California on April 13, 2014:
I really like hearing from people who have had the surgery both ways. I do fewer of these blocks as time goes on because our other forms of pain management have gotten better. Other blocks, like femoral for knee surgery, have a better benefit to risk ratio and I still do those quite a bit. Thanks for your valuable input.
Dennis Pinter on April 13, 2014:
Having had rotator cuff surgery twice, once with the block and once without. I would never again get the block. Too much risk of nerve damage.
The pain without the block was no big deal. Took very little pain pills afterwards. Besides. the pain only last for so long. Permanent nerve damage last for ever.
teamrn from Chicago on March 31, 2014:
I had never had an inter scalene block before, but I was going to have one when I had my shoulder surgery. Rather than ask my surgeon for infer, I got my info, elsewhere. Needless to say, I was petrified..
Well, I was given enough Versed and IV analgesics that I wasn't aware and all of a sudden my whole arm was numb. It was a piece of cake for me with no complications. But, I suppose Tahoedoc has seen her share and she's to be commended for writing such a good hub! Thumbs up! Annie
maria on March 30, 2014:
can it cause chronic cough?
Marcy Goodfleisch from Planet Earth on June 25, 2012:
Some acquaintances of mine were just talking about this type of surgery this weekend - and then I read your hub today! You always have such incredibly useful and informative hubs, and the topics are so important to us. Thank you! Voted up and up!
teamrn from Chicago on June 25, 2012:
I just know they couldn't do an epidural (?) because of hx of blood clot, but that TKR one was no fun; leg was numb for days, but shoulder numbness was gone in a day, I think!
TahoeDoc (author) from Lake Tahoe, California on June 24, 2012:
Haha - yes, you would have been awake/conscious (that's the standard of care, anyway). But, yes, versed is THAT good that you may not have any memory of the block being placed. I find that to be the norm and it is more unusual, although not a problem, for people to remember it.
The nerve block for the knee was a femoral block, most likely, with or without a sciatic block or other supplemental block.
teamrn from Chicago on June 24, 2012:
Tahoe, another well-explained procedure. On 2 occasions I had blocks: an inter scalene for a shoulder replacement and a nerve block for TKR. On neither occasion was I awake for the procedure; or was I? Versed is a wonderful thing; maybe I was aware, but don't remember it AT ALL. Is that possible?
Nettlemere from Burnley, Lancashire, UK on June 24, 2012:
I wouldn't like to be the one performing that nerve block injection. You must have cast iron control of your hands! Very interesting to read about and will hopefully remember some of it in case I'm ever offered one.
Dolphan5 from Warwick R.I on June 24, 2012:
Another insightful ,well written and informative article. I'm glad your on our side!
Thank You!